
Revolutionizing provider network management for payers
The only comprehensive solution for streamlined provider network management and operational bliss.
What we deliver
IMPROVED EFFICIENCY
By automating antiquated manual tasks to streamline workflows, CertifyOS significantly reduces the time and effort spent on credentialing. Providers are onboarded faster, leading to improved operational efficiency.
ENHANCED PROVIDER EXPERIENCE
CertifyOS simplifies the credentialing experience for providers. They can easily submit and track their application status through self-service portals, reducing administrative burden and enhancing satisfaction.
COST SAVINGS
The automation and efficiency provided by CertifyOS result in substantial and immediate cost savings. Health Plan partners have reduced administrative overhead, eliminated paper-based processes, and redirected resources to strategic initiatives.
































Better data, better operations
- Data First Architecture
- Automated Workflows
- Compliance Management
- Communication and Collaboration Tools
- Reporting and Analytics
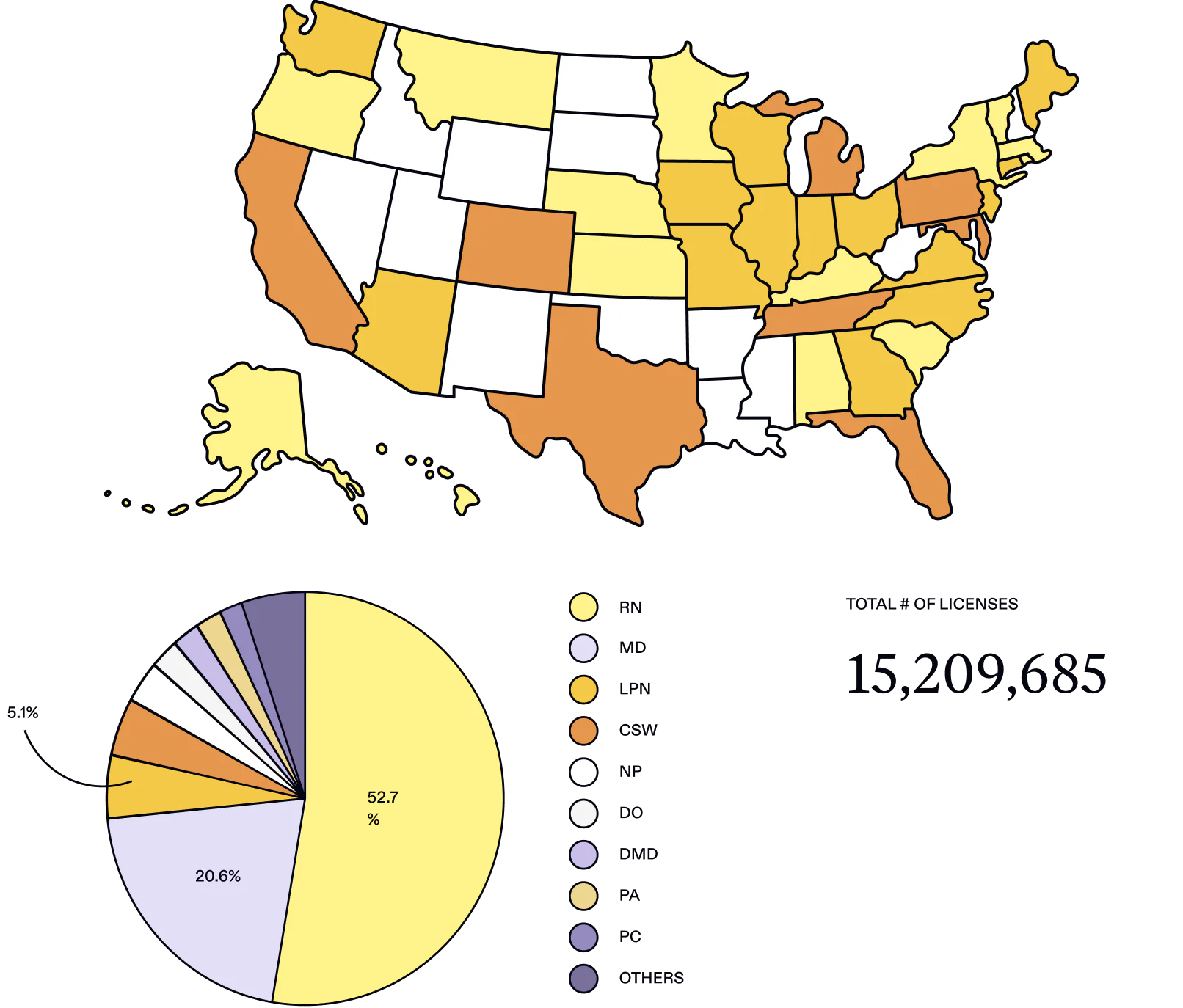
The most comprehensive coverage of any provider data source
HEALTH PLANS RESOURCES
- BlogCredentialing in healthcare is a complex, time-consuming process subject to frequent regulatory changes. Failure to keep up with the latest changes can result in significant penalties, including fines and disruptions to provider participation in health plans. Staying compliant requires continuous vigilance and efficient management practices.
- BlogOne of the biggest concerns for healthcare providers is the growing number of cybersecurity threats. In 2023, there were 739 healthcare data breaches reported in the USA alone, affecting over 136.1 million patient records. The average cost of these data breaches was estimated to be a whopping $7.13 million. Along with the financial losses, the data breaches affected the healthcare sector’s ability to deliver uninterrupted and satisfactory patient care.
One platform to get to the bottom of network management – and make a difference in your bottom line.

