AI Isn’t Going to Take Your Job, But It May Take Your Money… At Least for Now

We’ve all heard the headlines: AI is taking over because it’s better, faster, and cheaper than the human alternative. This may be true in some industries, but that’s not the case when it comes to healthcare. In fact, recent data paints a very different picture.
Recently, Certify brought together 65 leaders from health plans, venture firms, and large digital health companies for a first-of-its-kind provider data management summit, Blueprint, in New Orleans. At Blueprint, we heard from industry leaders and speakers on top-of-mind topics like AI in healthcare, data integrity, and the variables contributing to rising healthcare costs. Over the coming weeks, this blog will delve into what we learned across these sessions to continue thinking together about creating a better, more efficient healthcare system.
In one session, Christopher Kerns, the CEO of Union Healthcare Insights, helped set the stage for our attendees. He shared some of his team’s most recent data on the current state of the healthcare industry, including information on AI and its impact on healthcare costs.
One of the things that stood out to us during his session was the data he shared on rising healthcare costs and the opportunities that insurers and providers have to manage these costs. Kerns explained that he believes we are entering a new era of acceleration of healthcare spending and that innovations like AI can be efficiency drivers if managed strategically. Conversely, these variables can contribute to skyrocketing costs if not addressed in a way that’s both tempered and visionary.
The reasons for rising healthcare costs aren’t the same as they were twenty, ten, or even five years ago. Instead, innovations in AI, clinical technological advancements, and a rapidly aging population are leading to unexpected challenges for payers and insurers alike.
It’s not all bad news — there are opportunities for these players to work together to manage rising costs and implement high-tech infrastructure to power the future of healthcare. Below, we’ve highlighted six surprising variables Kerns believes lead to cost increases and shared insights into how payers and providers can find common ground to mitigate these variables.
Variable 1: AI Innovation
AI can (and likely will) drive healthcare savings in the future, but Kerns believes that it will take at least a decade for AI to catch up to the demands of our modern healthcare system. In our current state, rising input and innovation costs are burdening health systems with massive amounts of money, while buy-in from clinicians lags.
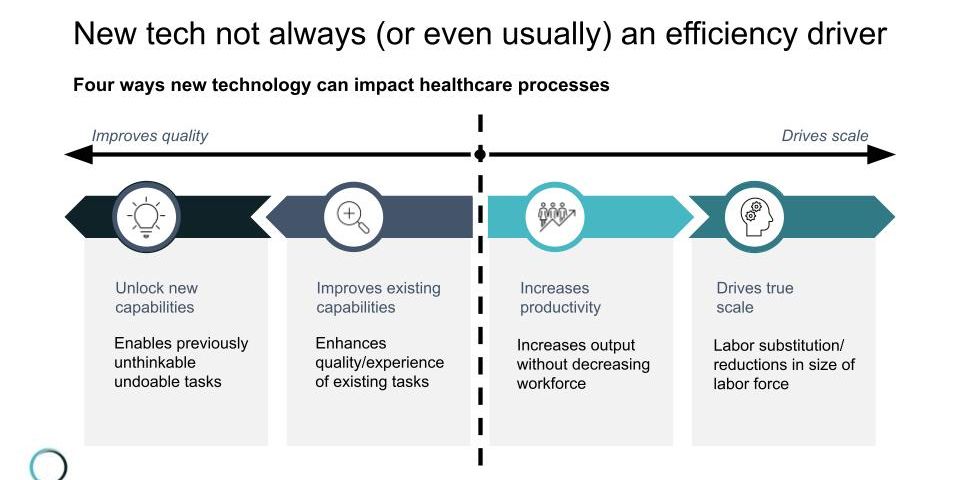
Despite what many say, new technology like AI isn’t always an efficiency driver. We’ve all heard that AI will take over millions of jobs in the coming years, saving companies millions of dollars. Instead, AI tends to be unwieldy and expensive, and problems with adoption and distrust make it a cost driver in the near term.
Still, appropriately implemented AI can lead to efficiencies. For example, Certify’s data-first platform provides a single AI-driven source of truth for provider data that can quickly become an invisible but indispensable way to drive cost savings.
Variable 2: Skyrocketing Administrative Costs
Healthcare administration costs are skyrocketing. Much of our administrative workforce uses outdated and unwieldy systems to manage large, complex healthcare systems. They do their best to digitize broken workflows or find narrow-point solutions to close gaps, but these are simply band-aids trying to repair a broken foundation.
Moreover, modern technology doesn’t always fill the gap. Many legacy systems fall short, and short-sighted additions of features or incremental improvements only add to the administrative burden, creating additional layers of work without addressing needed structural changes.
Healthcare needs a visionary administrative infrastructure that is tech-forward and mission-driven.
Variable 3: An Aging Population
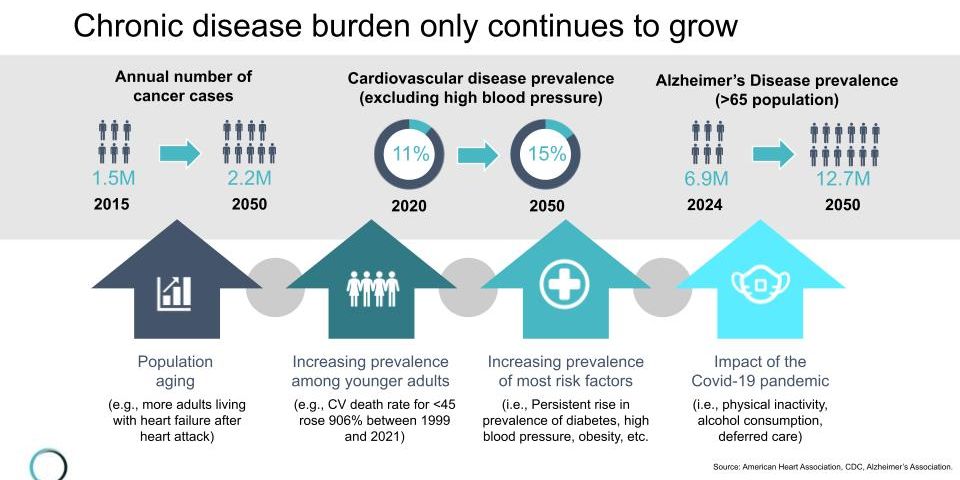
Our population is aging, and increased healthcare costs come with changing demographics. Older adults are at a higher risk for chronic diseases like cancer, cardiovascular disease, and Alzheimer's. For example, the number of cancer cases is expected to increase to 35 million by 2050 based solely on projected population growth, and increased disease burdens bring rising hospital and procedural costs. While we can’t do anything to solve for an aging population, we can look for ways to make healthcare more efficient to serve this population's needs.
One way healthcare systems have addressed this is by adopting innovative virtual-first plans that reduce in-person care and focusing on highly technical healthcare centers of excellence that can provide high-quality care at a lower cost.
Variable 4: Unwieldy Utilization
In recent years, healthcare utilization has increased across the board. Gaps in healthcare access, coupled with growing rates of chronic illness, have led to increased utilization of healthcare services, specifically expensive emergency care.
A small but noticeable shift has occurred from procedural to medical costs. Historically, highly profitable procedural costs, such as knee surgery or hip repair, have brought increased revenue into healthcare systems. Recent increases in the chronic disease load due to our aging population have skewed costs toward higher-cost, lower-profit medical expenses such as emergency room visits, hospital stays, and intensive care. This shift has decreased healthcare systems' margins and increased insurers' costs.
Variable 5: Pharmacy Spending Surge
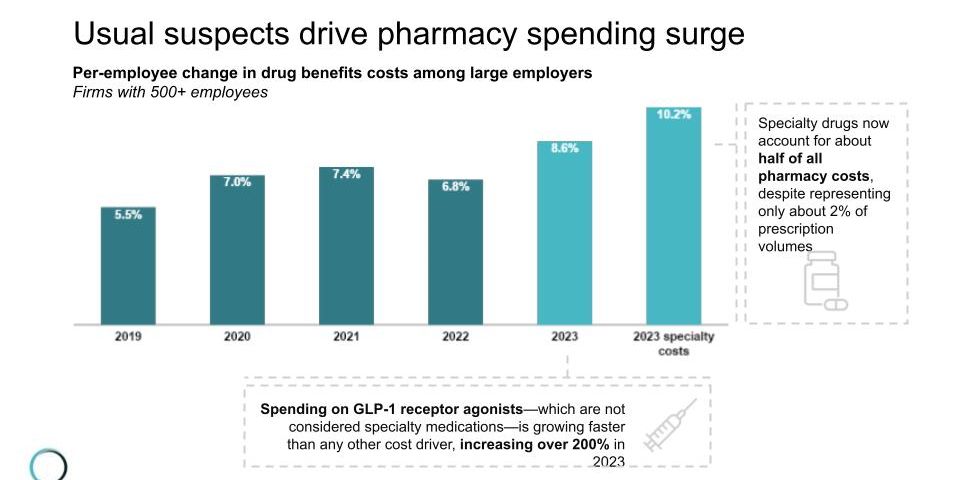
Innovations in pharmacology have given us new, highly effective options to treat disease. These specialty drugs have helped us manage chronic diseases like cancer and cardiovascular disease in a way that leads to much better health outcomes. Still, specialty drugs account for about half of pharmacy costs despite only representing a small fraction of prescriptions. These pharmacological advancements contribute to lower costs associated with chronic disease, but have led to a surge in pharmacy spending for many health plans.
On top of this, prescriptions for drugs in the GLP-1 agonist family have increased by more than 200% in the last year alone. These drugs are not considered specialty drugs, but the sharp increase in off-label use, coupled with long-term use patterns and side-effect-related emergency care, has made GLP-1s a huge cost-driver.
Variable 6: Workforce Expenses
Labor costs for the clinical workforce rose understandably during COVID-19. Frontline healthcare workers like doctors and nurses worked long hours in high-risk environments, which warranted higher compensation and better benefits.
Despite rising salaries, a long-predicted nursing shortage has come to fruition. Candidates aren’t moving into the industry as quickly as before, and increased personnel costs have made labor challenges one of the most significant cost drivers for health systems.
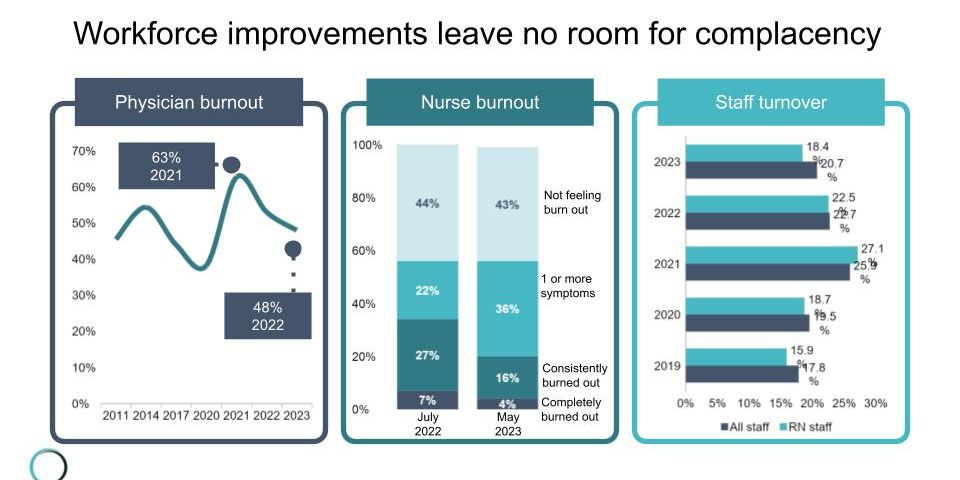
Additionally, administrative load is growing, and often the burden falls onto providers, taking hours of time and energy away from clinical work and leading to burnout and overload.
The Solution to Rising Costs
Administration is one of the core ways that healthcare systems, insurers, and employers can collaborate to lower costs. Many of the variables mentioned above drive costs in part due to clunky or outdated administrative systems. Likewise, AI inputs without proper education and implementation increase workloads and, at times, utilization.
In the next ten years, technology, specifically AI, will likely play a central role in healthcare at all levels. Your investments in the implementation and adoption of technology infrastructure today can drive cost savings in the future. Kerns recommends that payers and insurers invest in AI education for boards, leadership teams, and frontline staff, as well as enhanced security, data storage, and stewardship. By doing this, insurers and health systems can build the technology infrastructure needed to power future iterations of their models.
At Certify, our passion is finding ways to help payers and providers find common ground to reduce administrative costs and unlock more accessible care, lower costs, and a more efficient healthcare system. We sit at the nexus between bringing meaningful cost-savings to payers and helping providers continue to deliver top-level care.
To support these endeavors, Certify is working to reimagine the entire foundation of the administrative infrastructure for provider data. As a continuously updated, AI-verified source of truth powered by thousands of primary sources and available through one — yes, one — API, Certify can become an invisible but indispensable part of your solution to address rising costs.
No, your job isn’t going to be taken over by AI, but AI certainly can (and likely will) make your job more efficient, and be part of the solution to the pressures being felt around rising costs in our modern healthcare system.
To read more about the BluePrint Summit sessions, see 5 Key Takeaways on AI, Healthcare Costs, and Provider Data Management.
RELATED ARTICLES
- BlogEvery industry has its own “why hasn’t anyone solved this yet?” problem—the kind that sounds simple in theory but becomes remarkably complex at scale. Healthcare, unsurprisingly, has more than its share of these challenges.